Cardiovascular System
As we have seen in overview, Heart is a propelling pump which receives and distributes the blood to all cells through the tubes i.e. the blood vessels, to all cells in the body.
Let us see how this function is carried out.
This wonderful pump propels about 5 litres of blood every minute continuously till the end of life.
Structural and Functional aspect of Heart (Fig.1)
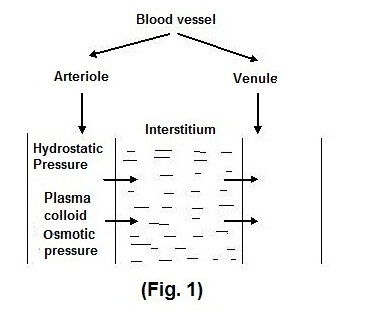
Left atrium contains oxygenated blood which is brought into it by pulmonary veins from lungs. When Left atrium contracts blood enters into left ventricle via mitral valve. Then left ventricle contracts and oxygenated blood is pushed into systemic circulation via aorta. Major arteries originate from aorta supplying blood to all organs. Remember, the capillary arising from smaller arteries ultimately pour out their contents in interstitial fluid which surrounds each cell. The cell takes up the required material including Hb which acts as oxygen carrier. Cell uses oxygen and other nutrients. It throws away carbon dioxide and other molecules in the interstitial fluid. Small venules take it up and ultimately the deoxygenated blood is brought to right atrium via SVC and IVC (Superior and Inferior vena cava) and Coronary Sinus. (Fig. 2)
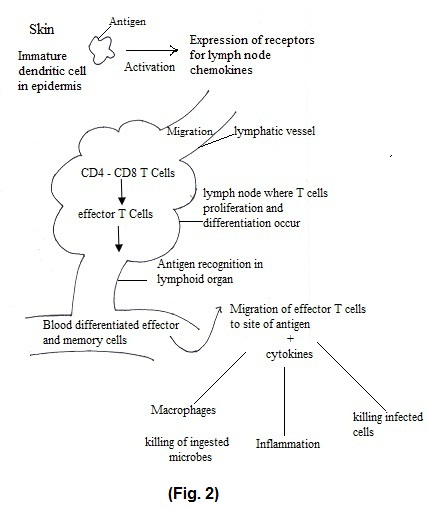
Now, the right atrium contracts and blood enters to right ventricle via tricuspid valve. Blood from right ventricle is ejected into pulmonary artery through pulmonary valve. When pulmonary valves open, because of pressure in right ventricle, this deoxygenated blood reaches lungs via pulmonary artery. Exchange of CO2 and O2 occurs in the alveoli. Then oxygenated blood reaches heart via pulmonary veins.
Let us discuss these events in detail.
For pumping of large quantity of blood, cardiac muscles require sufficient strength. Therefore, cardiac muscles are different from skeletal muscles as found in extremities. They are also different from smooth muscles as we find in Gastrointestinal tract. Besides Sodium Potassium (Na-K) pump, which is present in skeletal muscles, cardiac muscles receive additional energy from Calcium.
Another difference is the absence of cell boundaries in cardiac muscles. Due to this it acts like syncytium. It means, as if whole muscle contracts almost together.
Heart is composed of 2 syncytia
- Atrial syncytium
- Ventricular Syncytium
Therefore, both atria contracts together and both ventricles also contract at the same time.
Another important point to be noted is, atria have thinner wall as against ventricles because atria have to deliver blood to ventricles which are adjoining structures. Ventricles have thicker wall needed for stronger contraction. Obviously, ventricles have to eject blood travelling at greater distance and against high resistance like in aorta.
One more point to remember is that right and left ventricle simultaneously eject same volume of blood. However, left ventricular wall is relatively thicker than right ventricle because left ventricular blood travels to greater distance as against right ventricle, from where the blood reaches only up to lungs.
Between the right atrium and left atrium, there is a thin partition called as interatrial septum. Similarly, between right ventricle and left ventricle there is interventricular septum. At birth, there is an opening in the atrial septum called as foramen ovale. Generally, these opening closes soon after birth. If it does not close it produces congenital septal defects eg. Atrial septal defect.
As with most of the organ heart has covering called as pericardium. It consists of (1) Fibrous pericardium (2) Serous pericardium.
Serous pericardium forms double layer around heart called as parietal and visceral layer. Between these two layers there is a cavity called as pericardial cavity which contains pericardial fluid.
Let us study heart wall itself. (Fig. 3)
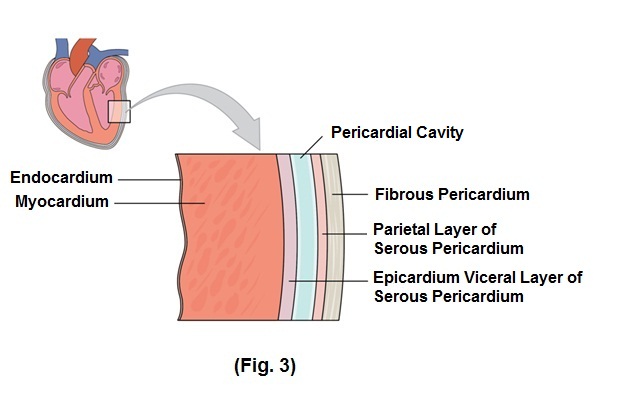
- Epicardium is inner visceral layer of serous pericardium.
- Myocardium is middle layer responsible for pumping action of heart and is composed of cardiac muscle tissue.
- Endocardium is the innermost layer which minimizes surface friction.
We will study cardiac valves.
Valves are there to ensure one-way flow of blood. These valves open and close in response to pressure changes as heart contract and relax.
- Tricuspid valve is present between right atrium and right ventricle.
- Between left atrium and left ventricle is bicuspid valve or mitral valve.
- The valve between right ventricle and pulmonary artery is called as pulmonary valve.
- The valve between left ventricle and aorta is called as aortic valve.
Pulmonary and aortic valves are called as semilunar valves because shape of these valves is like half-moon. From clinical point of view, narrowing of the heart valve opening is called as stenosis. Mitral valve stenosis is a condition which we commonly come across in practice, which occurs most of the time because of Rheumatic fever.
Conductive system of heart (Fig. 4)
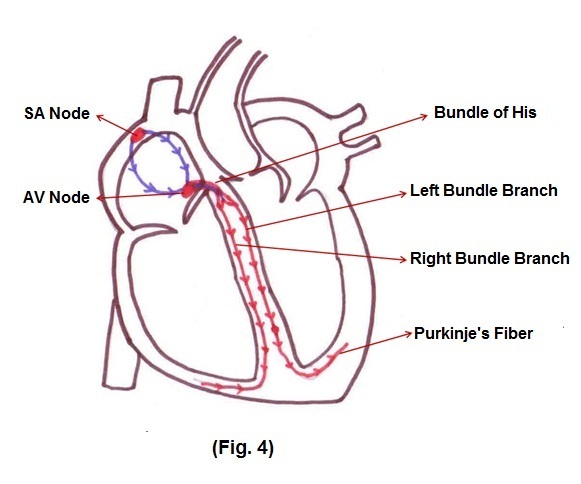
The activities of the heart are mainly controlled by conductive tissue. It is auto- rhythmic, in the sense that it automatically generates action potential at regular intervals. Sinus node controls heartbeat and is called as pacemaker of heart. Autonomic nervous system, especially parasympathetic and epinephrine secreted by adrenal medulla and sympathetic nerve ending, modify time and strength of each heartbeat by influencing SA node discharge. This rhythmical and conductive system of heart is susceptible to damage by heart diseases, especially ischemia from poor coronary blood flow resulting into arrhythmias.
Now we will study events associated with one heartbeat which is termed as cardiac cycle.
It is a time bound process. It consists of systole i.e. contraction, and diastole i.e. relaxation, of atria as well as ventricles.
Atrial systole -Just before atrial contraction starts, atrioventricular valves open. This occurs because pressure in ventricles is lower than atrial pressure at that moment in time. Therefore 80% blood directly passes to ventricles through atria even before atria contract. At this moment atrial contraction occurs, pushing remaining 20% blood into ventricles. These contractions occur due to firing by SA node and spreading of current through atria. This event occurs in 0.01 second. After this, action potential passes through AV node, right and left bundle branches and purkinje’s fibres. This initiates ventricular contraction, ready to rise in ventricular pressure, there by closure of AV valves. This closure of AV valve causes 1st heart sound, which we are able to hear. Increase pressure in both ventricles is responsible for opening of aortic and pulmonary valves. Ventricular contraction occurs in 0.03 second. Because of forceful ventricular contraction the blood is ejected into aorta and pulmonary artery. At the end of ventricular contraction, relaxation begins with sudden drop of ventricular pressure.
However, back flow of blood from aorta and pulmonary artery is prevented by closure of aortic and pulmonary valves. At this moment, we can hear 2nd heart sound. The time taken for ventricular relaxation varies from 0.03 to 0.06 seconds. During this period, the decrease in intraventricular pressure causes opening of AV valve which is a beginning of new cycle.
Now we will consider some terms which are important in relation to practice.
End diastolic volume — as term indicates it is the volume of blood in both ventricles at the end of diastole i.e. at the end of relaxation of ventricles. Normally, this volume is around 110 to 120 ml.
Stroke Volume — Amount of blood ejected from ventricle into aorta or pulmonary artery during each ventricular contraction. It is about 70 ml.
It means around 60% volume of blood is ejected during ventricular contraction which is called as Ejection fraction and it is usually equal to 60%. Decrease in ejection fraction occurs due to decrease in pumping capacity of heart.
Amount of blood ejected from ventricles will depend on
- The volume of blood in ventricle
- Resistance offered by Aorta and pulmonary artery
- Contractile capacity of heart muscle.
These factors either in isolation or in combination may contribute to various cardiac disorders.
Regulation of Heart Rate —
1. Autonomic Regulation of Heart Rate (Fig. 5)
Nervous system regulation of heart originates in the cardiovascular centre in medulla oblongata.
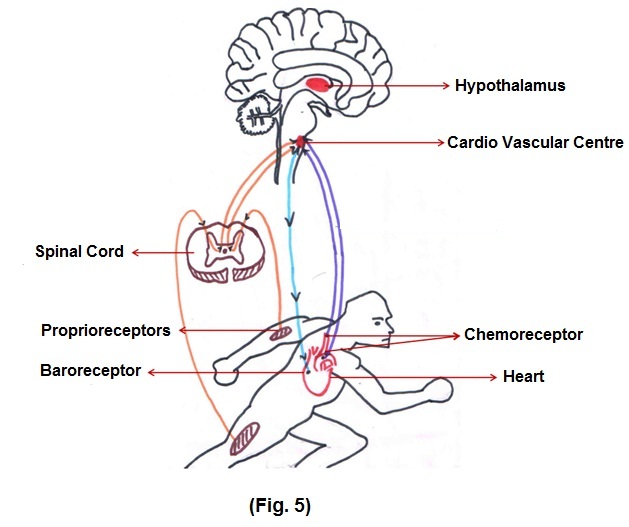
Cardiovascular centre (CVC) receives input from proprioceptors which are sensitive to movements of body, baroreceptors which are sensitive to pressure changes in blood vessels and chemoreceptors which are sensitive to CO2 and O2. Therefore, when we start running, message reaches to CVC via these receptors and heart rate goes up.
One more important point to remember is CVC receives input from higher brain centres like limbic system, hypothalamus and cerebral cortex. This is the reason that heart rate gets disturbed because of emotions, which originate from limbic system. Hormones like epinephrine and nor-epinephrine also have influence on Heart Rate.
Blood vessels — Blood vessels are like pipes which carry blood from heart to all cells. Aorta has to carry large amount of blood from the Heart. So, its size is larger than any other blood vessel.
As it proceeds, further division occur Arteries arterioles —— capillaries. (Fig. 2) Ultimately, blood supply to cell is through capillaries. However, between cells and capillaries there is interstitial fluid which acts as a medium for exchange of molecules between cells and capillaries. Another set of capillaries reunite to form
venules ——— smaller Veins ——— Larger Veins. Ultimately, the blood is brought to right atrium through Superior and inferior vena cava.
Blood vessels basically have 3 layers.
According to volume of blood which they have to carry, thickness of layers differs.
As compared to arteries veins have thinner layers. To facilitate the upward flow of blood from lower limbs veins have been provided with valves which prevent backward flow of blood. Besides that, contraction of limb muscles helps in pushing up the blood upward against gravity. Laxity of valves of veins will give rise to varicose veins especially in individual who stands for long time.
I would like to draw your attention to blood supply of heart.
It occurs through coronary circulation. One important aspect of coronary circulation is abundance of collateral circulation. It means alternative routes for circulation, which may be dormant. In atherosclerosis the chances of thrombus formation are quite high. Thrombus may obstruct any of the coronary artery leading to ischemic changes in the area of myocardium supplied by thrombosed vessel. In ordinary language it is called as Heart Attack. This is how this efficient pump may end up in catastrophe if we do not pay attention to exercise, diet and mental stress.
