Female Reproductive System
The main purpose of reproductive system is to form a new version of human being either male or female. Here we will study about the structures involved in the process of reproduction. (Fig. 1)
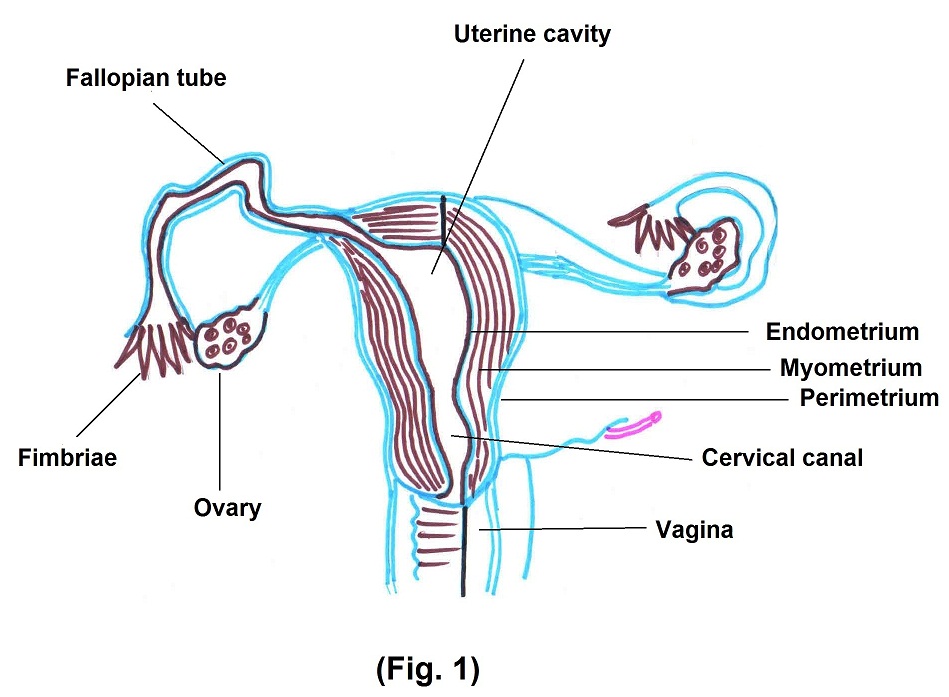
The principle organs of the female reproductive system are Ovaries, fallopian tubes, uterus, vagina, etc. Genital organs (collectively called as vulva), mammary gland is also included under the female reproductive system.
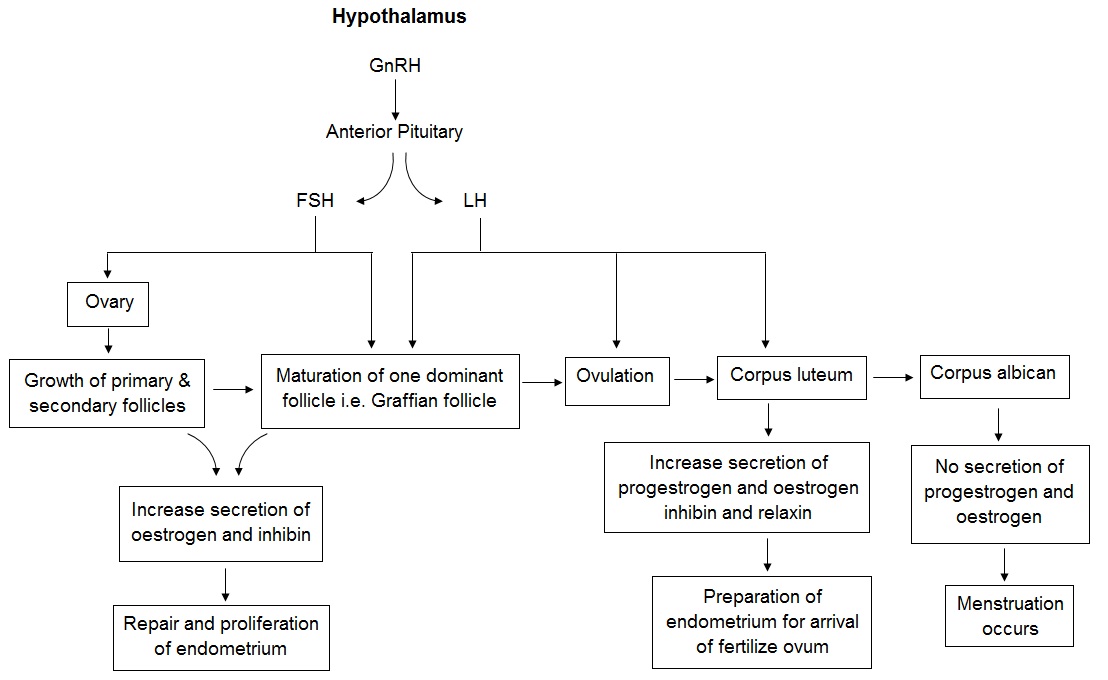
Now in brief we will study about each organ. There are 2 ovaries, one on either side of the uterus. They produce female gametes and hormones like progestrogen, oestrogen, inhibin and relaxin. At birth ovaries are populated with lifetime complements of eggs located in primordial follicles. At puberty, the hypothalamus starts pulsatile secretions of GnRH, resulting in activation of hypothalamus – pituitary – ovarian – uterine axis. FSH and LH secreted by anterior pituitary gland stimulate the growth of few primordial follicles during each month. Out of this, only one follicle begins to outgrow and becomes dominant i.e. graffian follicle while other follicles involute, this process is called atresia. (Fig. 2)
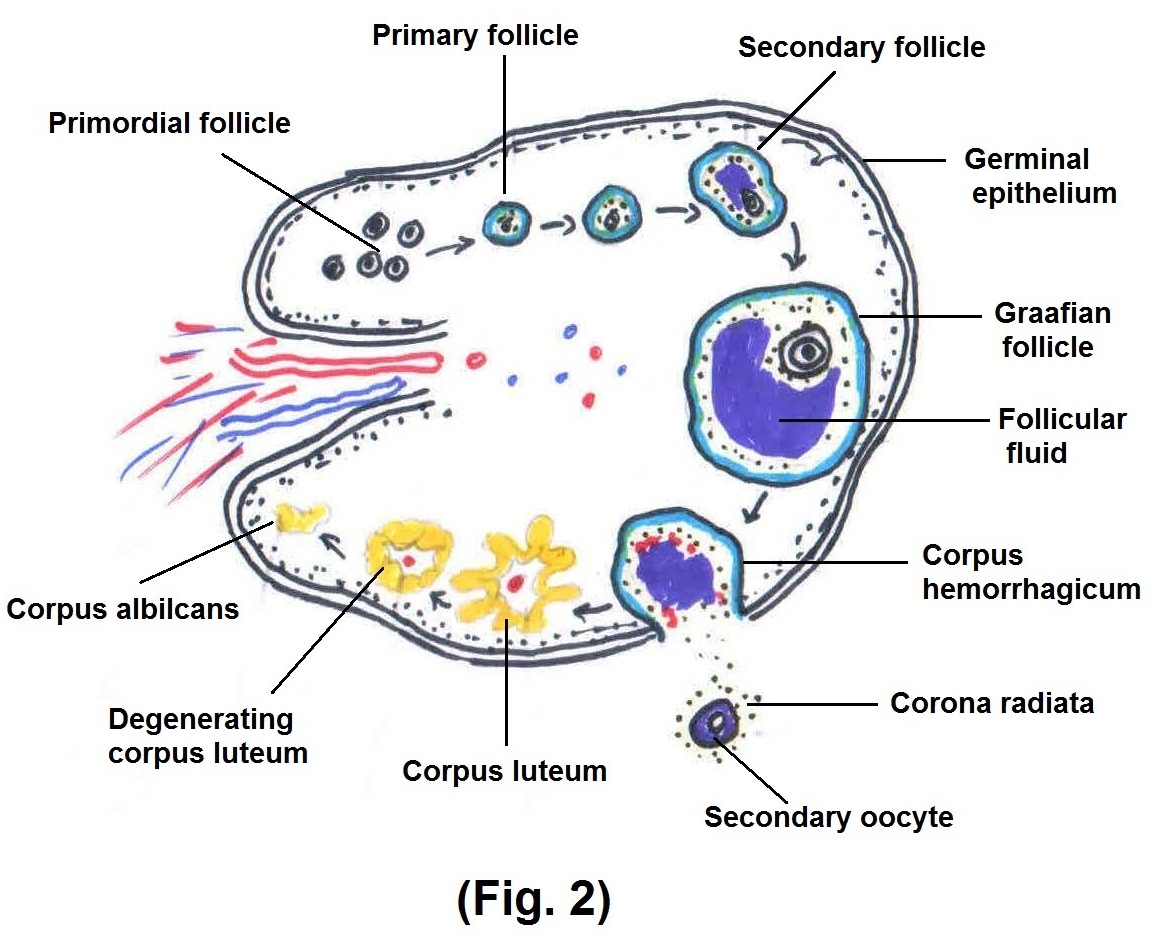
This is important because it allows only one follicle to ovulate during each month, thus prevents more than one child from developing with each pregnancy. During ovulation time graafian follicle ruptures and ovum is released into the pelvic cavity. After the release of ovum, it is immediately pick up by the fimbrial ends of the fallopian tube & travels forward towards the uterus.
The time of ovulation is always between 13 and 15 days before the next succeeding menstrual cycle. Knowledge of ovulation time is important in the control of fertility, artificial insemination.
If during ovulation time, ovum comes in contact with the sperm, it gets fertilized. Normally the fertilization takes place in the distal portion of the fallopian tube i.e. ampulla and the ovum are subsequently transported by the contractions of the tube into the uterine cavity. Fallopian tube contains ciliated and non ciliated cells, which help the ovum to propel forward and provides nutrition. The journey takes 6 – 7 days to reach the uterine cavity. In pathological conditions, implantation may occur anywhere outside the uterine cavity, called ectopic pregnancy.
Unless fertilized, ovum does not survive for more than 24hrs and it degenerates into the fallopian tube.
In the uterus fertilized ovum gets implanted and further development of the foetus starts. Uterus consists of 3 layers of tissue like perimetrium, myometrium and inner one endometrium, (Ref. fig.1) which is a highly vascularized layer. Endometrium is divided into 2 layers, stratum functionalis which lines the uterine cavity, and which sloughs off during menstruation. Second layer is stratum basalis which is the permanent deeper layer. Extensive blood supply to the uterus is essential to support the regrowth of stratum functionalise after menstruation, implantation of fertilized ovum and development of placenta.
Cervix produces mucus which is normally viscous and forms a cervical plug that inhibits sperm entry into uterus. During or near ovulation time cervical mucus become less viscous and more alkaline, which helps the sperm to enter into the uterus.
Vagina is lined by mucus membrane; mucosa contains large stores of glycogen, decomposition of which produces organic acids that retards the microbial growth.
Now we will discuss about the puberty, puberty is the slow process involving several years during which the physical growth and secondary sexual characters develop to maturity and the menstruation is developed. Normally puberty begins after 8 years of age. If it occurs before the age of 8 years, it is termed as precocious puberty. This occurs due to premature activation of the intact hypothalamus – pituitary — ovarian axis. Delayed puberty may be familial or idiopathic. Puberty is delayed as long as 5 years, after that it requires investigation. The age for the onset of menarche is between 11 to 13 years.
Until puberty, hypothalamus and anterior pituitary gland are under are some inhibitory influences of a higher brain centre. At puberty this inhibition is gradually withdrawn, and the hypothalamus starts secreting GnRH and under the stimulus the GnRH, pituitary gland releases FSH and LH, as well as growth promoting hormone. This growth promoting hormone causes a spurt in the height. Now we will discuss the hormonal interaction in the ovarian and uterine cycle.
Normally menstrual fluid is non-clotting because a fibrinolysis is released along with endometrial contents. Menstrual irregularity indicates an underlying abnormality like
1. Amenorrhoea — absence of menstrual periods. Menstruation is dependent on chain made up of hypothalamus – pituitary- ovary- uterus; breakup in this link may lead to amenorrhoea. Also, psychological causes are also responsible.
2. Dysmenorrhoea – Refers to the crampy abdominal pain. Many of the cases subside after proper diet and exercise, but in some cases underlying pelvic pathology like endometriosis, adenomyosis should be ruled out. Endometriosis is the occurrence of ectopic endometrial tissues outside the cavity of the uterus. It is the disease of childbearing age.
3. Menorrhagia — In this case, menstrual cycle is unaltered, but the duration and quantity of menstrual loss are increased. Causes may be some general disease like leukaemia, thyroid dysfunction or local causes like uterine fibroid or IUCD.
4. Metrorrhagia — In this case, there is irregular, acyclic bleeding, from the genital tract. Bleeding may be intermittent or continuous. It is a primary symptom of genital tract neoplasm.
5. Polymenorrhea — In this condition, cycle is reduced from the normal of 28 days cycle to a cycle of 2 to 3 wks. It is characteristically seen at the time of menarche and menopause. Also, conditions like salpingo-oophoritis, chronic PID, fibroids may cause this condition.
6. D.U.B. (Dysfunctional uterine bleeding) — In this entity aetiology is purely hormonal and pelvic examination is normal.
Menopause is the time at which menstruation ceases, it occurs between the ages of 45 to 55 years. Late menopause is common in women suffering from uterine fibroids and endometrial carcinoma. During climacteric time ovarian activity declines, menstrual cycles become anovulatory, irregular and afterwards menstruation ceases. Genitalia undergo atrophy. Osteoporosis, hot flushes, arthritic changes occur in the joints, mental depression, dysuria, hirsutism are some of the common menopausal symptoms.
Now we will discuss about the female sexual act. Stimulation of the female sexual act depends on psychological factors and local organs stimulation. Sexual sensory signals are transmitted to the sacral segments of the spinal cord through the pudendal nerve and sacral plexus, and through this they are transmitted to the cerebrum.
In the early phases of sexual stimulation parasympathetic signals dilate the arteries of erectile tissue, which is around the introitus up to the clitoris, which allows rapid accumulation of blood in the erectile tissue, so that introitus tightens around the penis, this helps the male partner in attaining sufficient sexual stimulation for ejaculation to occur. Parasympathetic signals also cause the bartholin glands to secrete mucus, which provides lubrication during act. Also, vaginal epithelium secretes much of the mucus and provides lubrication. This lubrication is necessary during act to establish a satisfactory massaging sensation.
